Excretory System Definition
The excretory system consists of the organs that remove metabolic wastes from the body. In humans, this includes the removal of liquid nitrogenous waste in the form of urine, and solid wastes especially from the breakdown of hemoglobin. The removal of urine is accomplished by the urinary tract, while solid wastes are expelled through egestion from the large intestine.
Functions of the Excretory System
The excretory system functions as the bulwark and balance to the digestive system. While we consume food and drink to nourish the body and provide energy, the excretory system ensures that homeostasis is maintained, irrespective of changes to the nutritive value of food.
It regulates the fluid balance of the body, maintaining adequate salt and water levels. When there is excess water, it is removed through the production of hypotonic urine. When we consume salty food, or lose water through perspiration, the concentration of urine is increased, to preserve the osmolarity of body fluids.
The excretory system, especially the urinary tract, is necessary for preventing the toxic build up of nitrogenous wastes, such as ammonia or urea.
The kidneys secrete a hormone called erythropoietin that induces the bone marrow to produce more red blood cells.
Excretory System Organs
The primary excretory organs in the human body are the kidneys, ureters and urinary bladder, involved with the creation and expulsion of urine. Through these organs, much of the nitrogenous waste of the body, especially urea, is expelled. Other organs such as the liver, large intestine and skin are also necessary for the excretion of specific metabolic wastes.
Kidneys
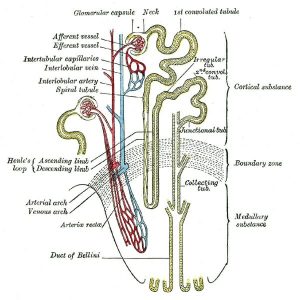
The kidneys are paired, bean-shaped organs located in the abdomen, on either side of the spine, under the diaphragm. They are made of a large number of structural and functional subunits called nephrons. These nephrons perform the primary task of filtering blood and removing waste products. Each nephron snakes between the outer cortex of the kidney and the inner medulla, with different activities occurring at each site.
The image shows parts of two nephrons, with their relative positions within the kidney. Each nephron begins with a globular structure called the Bowman’s capsule located in the renal cortex. This structure receives blood from renal circulation through an afferent arteriole that further divides to form a tuft of capillaries called the glomerulus. Unusually, these capillaries come together to form the efferent arteriole instead of a venule. The kidney is richly vascularized with capillary beds surrounding each nephron (intertubular capillaries) as well as blood vessels running between the lobes of the kidney (interlobular arteries and veins).
A process of ultrafiltration creates the glomerular filtrate from blood, which is remarkably similar in composition to blood plasma. Water, small molecules, and proteins smaller than 30 kilodaltons in size can pass freely into the lumen of the Bowman’s capsule.
The Bowman’s capsule involutes and creates a neck, which then extends into the first elongated tubular structure called the proximal convoluted tubule or PCT. The PCT is the site for secreting some acids, and for reabsorbing nearly two-thirds of the glomerular filtrate. It also removes all glucose and amino acids. The presence of either glucose or other organic solutes in the urine is a sign of kidney damage, especially of the cortex. Some nitrogenous waste is also removed from the body as ammonia secreted from the cells forming the PCT. Many medications are also detoxified at this site.
The PCT leads into an U-shaped structure called the Loop of Henle, extending into the medulla of the kidney. This has two functionally and anatomically distinct arms – the ascending and descending limbs. Between these two arms of the loop of Henle, through a set of electrolyte pumps, a high urea concentration is maintained in the medulla of the kidney.
The PCT initially leads into the descending loop, which is freely permeable to water and mostly impermeable to ions – especially urea. The high osmolarity of the medullary region of the kidney draws water out the descending loop, allowing the urine to become concentrated.
This is followed by the thin ascending loop, which has the opposite property of being permeable to ions and impermeable to water. Solutes such as sodium ions are actively reabsorbed, reducing the concentration of urine. However, by this time, the volume of fluid filtered at the glomerulus has been reduced to a fraction of its quantity.
The ascending limb then leads into the distal convoluted tubule or DCT, also known as the second convoluted tubule. The DCT is the site for the activity of most hormones that regulate kidney function. This includes antidiuretic hormone (ADH) and angiotensin II (AT II). This region regulates ion and pH balance. From the DCT, urine passes through collecting ducts that finally lead out of the kidney through ureters.
This image is a composite representation of the nephron, with details about the substances reabsorbed at each site, the osmolarity of the filtrate at different parts of the nephron, and the impact of different hormones or medications.
Urinary Bladder
The urinary bladder is a sac-like structure with muscular walls that holdS urine until it is expelled from the body during micturition. The bladder receives urine through two ureters – one from each kidney –that enter through openings called ureteric orifices. These orifices are located at the convex fundus of the organ. Urine exits the bladder through the urethra.
The walls of the bladder are made of smooth muscle and the inner epithelial lining of this organ consists of a remarkable tissue called transitional epithelium. The cells of this stratified tissue change shape based on whether the bladder is empty or full, allowing it to remain elastic, accommodating up to half a liter of urine.
In men, the bladder lies on the pelvic floor in front of the rectum. In women, it is located near the uterus, leading to a number of changes to the patterns of micturition during the course of pregnancy. During the course of gestation, there are major changes to blood volume and increases in glomerular filtration rate. While the bladder itself increases in size, nearly doubling by the end of the third trimester, the enlarged uterus with the weight of the fetus, amniotic fluid, placenta and other tissues can create stress incontinence.
Liver
The liver is the main detoxifying organ of the body, especially for nitrogenous wastes. The cells of the liver play host to biochemical processes that create ammonia from amino acids. Since ammonia is extremely toxic, it is quickly converted to urea before being transported in the blood towards the kidney.
Most animals make the choice between ammonia, urea and uric acid as the preferred mode for nitrogenous waste excretion, based on the availability of water. While ammonia is toxic, it can be quickly diluted and removed from the body, and therefore remains the chemical used by aquatic animals. Terrestrial animals with regular access to water tend to use urea, which has lower toxicity. Birds and other animals that have minimal water intake expend energy to convert urea into uric acid.
Large Intestine
The liver is also necessary for the removal of the decomposed hemoglobin, some drugs, excess vitamins, sterols and other lipophilic substances. These are secreted along with bile and finally removed from the body through feces. The large intestine therefore plays a role in excretion, especially for hydrophobic particles.
Skin
The skin is a secondary excretory organ, since sweat glands in the dermis can remove salts and some excess water. The skin also has sebaceous glands that can secrete waxy lipids.
Diseases of the Excretory System
The excretory system, especially the kidneys, can be injured, damaged or have suboptimal functioning, either due to acute stress or through chronic conditions.
Renal Failure
Renal failure or renal insufficiency is the inability of the kidney to filter wastes from the blood and maintain fluid homeostasis. The causes for renal failure could be diseases such as diabetes mellitus and hypertension that can cause damage to glomerular capillaries. Diabetes insipidus arising from hormonal insufficiency, reduced blood flow from injury to the vasculature of the kidney, infections in the body and blood stream, medications or kidney stones can also affect kidney efficiency.
Initial symptoms can be as mild as swelling in the legs, indicative of the inability of the kidney to maintain fluid homeostasis. The presence of toxins in the blood can cause a feeling of nausea and vomiting. Changes to the RBC metabolism and reduced erythropoietin secretion from the kidney can lead to anemia, weakness, sleepiness, and confusion. Excessive potassium ions can lead to cardiac arrhythmias, and changes to muscle tone and contractility.
Depending on the cause for renal insufficiency or failure, the injury could be reversed. In most cases, long term changes to diet and lifestyle are necessary to maintain health. When the kidney is functioning at extremely low efficiency, waste removal has to be done through an external apparatus, called the dialysis machine. Kidney transplant is also occasionally recommended.
Excretory System Facts
- The urinary bladder can hold up to 600 ml of liquid. During early pregnancy, the uterus presses on to the bladder, creating a greater frequency of micturition.
- Most of the amniotic fluid surrounding the growing fetus is fetal urine, though its composition is very different from normal urine. The bladder of the fetus begins to empty around the 10th week of gestation.
- This fetal urine and the amniotic fluid are actually important for the development of fetal lungs.
- The white parts in bird excreta are composed mostly of uric acid.
- The brownish pigmentation of feces mostly derives from bile salts.
Related Biology Terms
- Fundus – Part of a hollow organ, such as the bladder or stomach, farthest from its opening.
- Kilodalton – Unit of molecular mass, representing the mass of a thousand protons or neutrons.
- Micturition – Expulsion of urine from the bladder. Mostly a voluntary activity initiated by the relaxation of the urinary sphincter.
- Ultrafiltration – Membrane-based filtration that allows for selective removal of solutes and particles, usually powered by fluid pressure or concentration gradients.
Quiz
1. Which of these statements about the excretory system is true?
A. Ammonia is converted to urea in the kidney
B. Uric acid is commonly used as the excretory molecule in aquatic animals
C. Urea is generated in the liver and filtered from blood in the kidney
D. All of the above
2. Which of these statements about a nephron is NOT true?
A. Each nephron has segments in the renal cortex and renal medulla
B. Nearly one-third of the water and solutes of the glomerular filtrate are reabsorbed in the PCT
C. The descending loop of Henle is impermeable to solutes
D. Antidiuretic hormone and angiotensin II act on the DCT
3. If albumin, with a molecular mass of 66.5 kilodaltons is found in urine, what might this indicate?
A. Glomerular capillaries are damaged
B. PCT is not functioning properly
C. Dehydration
D. Renal medulla is injured
Excretory System

No comments:
Post a Comment