Definition of Pituitary Gland
The pituitary gland, also known as hypophysis, is a diminutive, pea sized gland located at the base of our brains. It is commonly referred to as the “master gland” of the human body, as it releases a ton of hormones that circulate our system and aid in maintaining our internal homeostasis. Moreover, the pituitary gland is also the “master” or dominant gland controlling the activity of other glands, as well. The pituitary gland is both responsible for producing and storing an assortment of important hormones that we will discuss in more detail.

The image is an illustration of the pituitary gland as it is situated in the human brain. The depiction shows its relative size.
Pituitary Gland Location
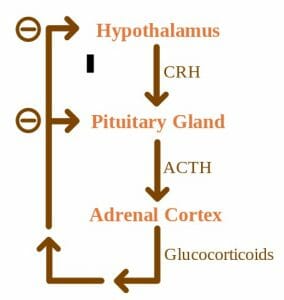
The pituitary gland lies roughly in the center of the human skull. It rests below the hypothalamus of the brain and behind the bridge of our noses. Its setting actually makes sense, in light of the hypothalamus’s role in fine tuning the activity of the pituitary gland. This is made possible by the nerve fibers that span these two structures and allow for easy communication. Likewise, a thin vascular connection that is forged within the pituitary stalk, or infundibulum, facilitates the hypothalamus’s control. Further, the pituitary gland itself is supplied by branches off of the internal carotid artery. Its regulation is fine-tuned by a negative feedback relationship between the pituitary and hypothalamus.
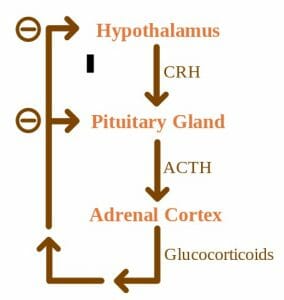
The concept map illustrates the complex regulatory relationship between the superseding hypothalamus and the pituitary gland. The relationship follows a negative feedback loop.
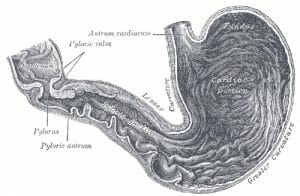
Structurally speaking, the pituitary gland is notably parsed into three sections: the anterior (front), intermediate, and posterior (back) lobes. Each can be described according to their unique functions. The anterior lobe has primary roles in the development of the human body. This involves secreting hormones that orchestrate our reproduction and sexual maturation. These hormones will control growth as well as activate the adrenal and thyroid glands and sexual organs. The intermediate lobe will secrete hormones that stimulate the cells in our body that produce pigment, called melanocytes. These melanocytes are the reason there is such a variation in our skin color. Lastly, the posterior lobe makes ADH, which is the hormone that allows our kidneys to reabsorb water into the bloodstream to prevent dehydration. Oxytocin is also made in the posterior lobe and will induce contractions during childbirth. While these hormones are supremely important to our species’ survival, they are few among the many hormones made by the pituitary gland.
Pituitary Gland Function
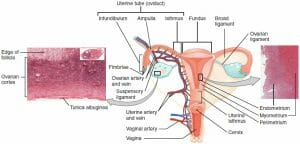
The main function of the pituitary gland lies in its ability to make hormones that retain many of our bodily functions. The front and back lobes are the primary secretory glands. As discussed before, the posterior lobe secretes oxytocin and ADH. Oxytocin not only stimulates uterine contractions to facilitate birth but also causes breast tissue to make milk, in preparation of caring for a child. The anterior pituitary gland has a bigger roster of hormones. It produces prolactin, which like the posterior’s oxytocin will trigger milk production post-partum. Follicle-stimulating hormone (or FSH) is released to stimulate sperm production and egg maturation in women that are able to produce estrogen. Likewise, luteinizing Hormone (LH) will stimulate testosterone release in men and egg release in ovulating women. One of the most important products of the anterior lobe is thyroid-stimulating hormone (TSH). The thyroid helps coordinate metabolic activity, and likewise, the TSH will stimulate thyroid activity. Therefore, TSH indirectly allow the thyroid to assume all of its roles. Adrenocorticotropic (ACTH) is released as well and will stimulate the creation of stress hormone, cortisol. Cortisol is essential to our survival and will keep our blood pressure and sugar levels at a healthy normal – of course, in healthy amounts. Any over or under expression has negative consequences. Lastly, the anterior pituitary lobe also releases growth hormone (GH), which is responsible for the muscle and bone mass growth that occurs during development. When growth is unaccounted for, as with a dysregulation of GH production, it can lead to serious illness, if not cancer as we will discuss below.
Posterior Pituitary Lobe:
Anterior Pituitary Lobe:
- Prolactin
- Follicle Stimulating Hormone (FSH)
- Luteinizing Hormone (LH)
- Thyroid-Stimulating Hormone (TSH)
- Adrenocorticotropic (ACTH)
- Growth Hormone (GH)
Pituitary Gland Disorders
Deficiencies in any of the hormones mentioned above can cause illness, which vary in gravity. Starting with the posterior lobe, a deficiency of ADH will increase our thirst and urination. A lack of prolactin will quite predictably lead to an inability to lactate, which to this day cannot be treated. TSH deficiency has symptoms similar to those from a compromised thyroid gland, which includes fatigue, memory loss, and bodily weakness. A lack of LH or FSH will result in a decrease in libido, irregular menses, erectile dysfunction, and mood changes. ACTH deficiency will cause nausea, body aches, poor appetite, and even low blood sugar and pressure. Lastly, deficiency growth hormone will lower muscle mass and bone density, which has long term ramifications on the quality of our lives.
An overproduction of hormone has its own consequences. Too much growth hormone can lead to gigantism and acromegaly, or too much growth of bones and soft tissues leading to heart issues and sleep apnea. Too much TSH will result in shakiness, irritability, and high blood pressure. Too much prolactin will cause inappropriate expression of breast milk that can occur in women or men, and a weakening of bones. Excess ACTH will cause weight gain among brittle bones and mood instability. Lastly, excess FSH and LH are linked to infertility and irregular menstruation.
The most common type of pituitary gland disorder, however, are tumors. The grand majority of pituitary tumors are benign, or just a noncancerous swelling in the gland that may not cause any symptoms and may never be symptomatic. Unlike many types of tumors, most people afflicted with pituitary tumors have no prior family history of issues with the pituitary gland and is not usually genetically inherited. One of these exceptions is multiple endocrine neoplasia (or MEN) which is a set of inherited disorders that lead the body’s endocrine glands, including the pituitary gland, to overexpress hormones. But pituitary tumors, specifically, still remain by and large benign.
Tumors on the Pituitary Gland
Various types of pituitary tumors exist. In general, people with a pituitary gland tumor will experience a series of telltale symptoms. Most will have vision problems, headaches, menstrual changes, infertility, mood changes, fatigue, and even Cushing’s syndrome – which has its own set of symptoms including, but not limited to, high blood pressure and weight gain secondary to too much ACTH release.
The most common type of pituitary tumor is called a “non-functioning” tumor. The name derives from its inability to make hormones. These patients will have issues with their vision and headaches. Furthermore, pituitary tumors can be divided into three groups according to their problematic actions.
Hypersecretion refers to the making of too much hormone, and this is an issue afflicted by a secretory pituitary tumor. Hyposecretion, in contrast, is too little hormone production and is normally caused by a large pituitary tumor that will physically block the pituitary gland from making hormone. It can also result from surgical resection of a tumor. Lastly, tumor mass effects are the issues that arise from a growing pituitary tumor that is pressing against the pituitary gland and may result in compromised vision and headaches, as well.
Other pituitary conditions worth noting include craniopharyngioma. This is a type of cyst or tumor that is congenital, meaning it is present at birth. It can swell and fill with fluid, and may cause headaches and vision issues as well as sleep issues. ESS, or empty sella syndrome is a disorder that arises from an affliction in the bony structure that encases the brain and surrounds the pituitary. A primary ESS will be a small defect that give rise to high pressure in the bony base that causes the gland to flatten. This is linked to high blood pressure and obesity in females. On the other hand, secondary ESS will result from surgery or an injury that has caused the pituitary gland to regress. The symptoms will be related to pituitary function loss, such as infertility and fatigue.
Quiz
1. Which of the following is released by the posterior pituitary?
A. Prolactin
B. ACTH
C. Oxytocin
D. Growth Hormone
Answer to Question #1
C is correct. The posterior lobe releases hormones oxytocin, involved in lactation and uterine contractions, and ADH which is not listed in these choices. The other choices are hormones released from the anterior pituitary lobe.
2. Match the correct symptom with a deficiency in ACTH, per the article:
A. Erectile dysfunction
B. Nausea
C. Thirst
D. Reduced muscle mass
Answer to Question #2
B is correct. An ACTH deficiency has several symptoms, including body aches, poor appetite, and nausea. The other options listed are associated with deficiencies in the other pituitary hormones.
3. Match the correct symptom with an overexpression of LH, per the article:
A. Infertility
B. Weakened bones
C. Weight gain
D. Acromegaly
Answer to Question #3
A is correct. The other choices listed are correctly symptoms of hormone overexpression. But infertility is the only symptom related to LH and FSH overexpression. The others are associated with the overexpression of ACTH (weight gain), GH (acromegaly), and prolactin (brittle bones).
References
- Hormone Health Network. “Pituitary Disorders.” Hormone Health Network. Retrieved on 2017-07-28 from http://www.hormone.org/diseases-and-conditions/pituitary
- Cancer Editorial Board (2016). “Pituitary Gland Tumor: Syptoms and Signs.” Cancer.Net. Retrieved on 2017-07-29 from http://www.cancer.net/cancer-types/pituitary-gland-tumor/symptoms-and-signs
- Health Line Medical Team (2017). “Pituitary Gland.” Health Line. Retrieved on 2017-07-28 from http://www.healthline.com/human-body-maps/pituitary-gland
- Pituitary Foundation (2017). “What is the pituitary gland?” Pituitary. Retrieved on 2017-07-29 from https://www.pituitary.org.uk/information/what-is-the-pituitary-gland/
Pituitary Gland